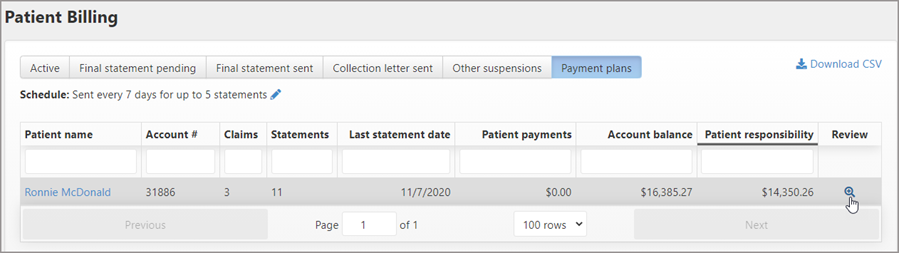
Using Review on Patient Billing Page
To use review the Patient Billing Page:
-
On the navigation bar, click Claims > Patient Billing.
-
Click the Active tab and then find the patient name on the list. If the list is long, start typing the name in the box under the Patient Name heading.
-
Click the Review icon
 under the Review column. This page will help you to determine the best way to deal with the account. It shows the patient’s propensity-to-pay, current patient responsibility, running balance, and statement details.
under the Review column. This page will help you to determine the best way to deal with the account. It shows the patient’s propensity-to-pay, current patient responsibility, running balance, and statement details.
With the exception of the "Final statement sent" and "Other suspensions" tabs, the Review window displays the same information regardless of which tab you are on. You can suspend the account, edit the reason for the suspension, remove the suspension, and send another statement.
The Review window contains the following tabs:
Patient responsibility tab
This tab displays when you review an account on the Patient Billing page and on the Account page.
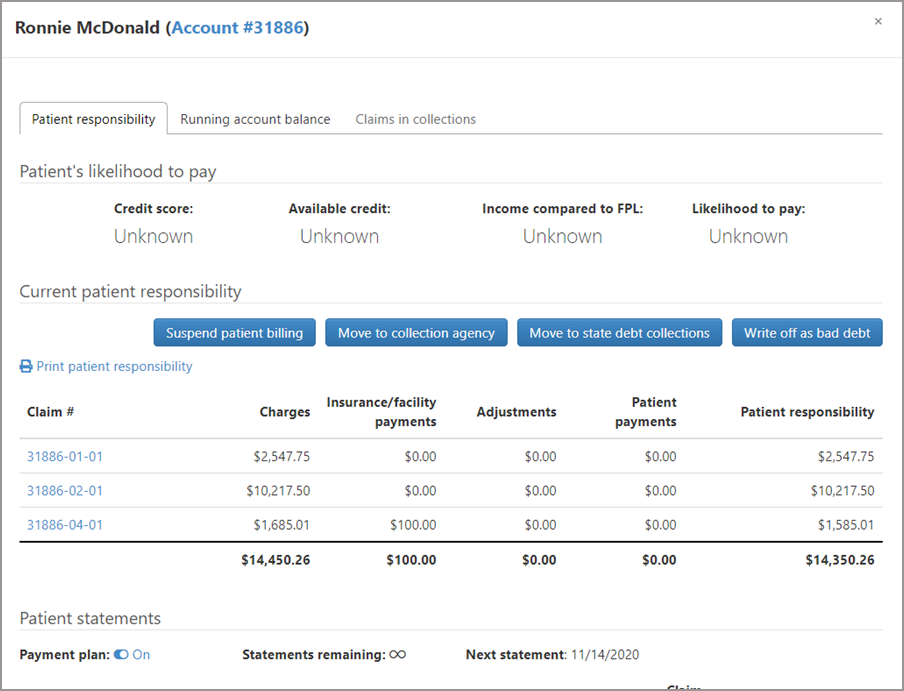
Patient’s likelihood to pay

Likelihood to pay runs automatically when the patient is new, when the claim moves to Patient Billing, and when a user accesses the Patient Billing page. You can also run it from this window by clicking the Check likelihood to pay button. The results of the likelihood to pay query is divided in four categories, credit score, available credit, income compared to federal poverty level, and likelihood to pay.
The Federal Poverty Level (FPL) is used to measure a household's poverty status. This level can help determine if the individual can qualify for Medicaid.
The likelihood to pay value is derived from the credit score:
- Low: Credit score 0 – 500
- Medium: Credit score 500 – 600
- High: Credit score over 600
Patient responsibility
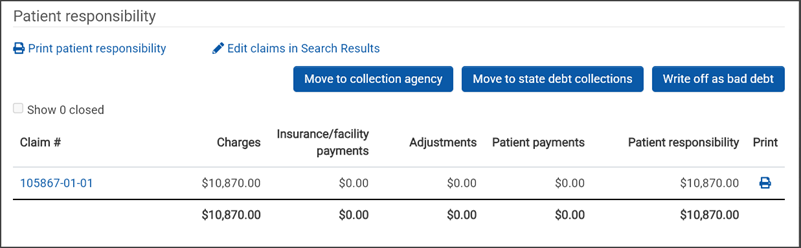
This section lists the claims with the resulting payments that the patient is responsible for.
At the top of this section there are two links:
-
Print patient responsibility: Click this link to generate a patient invoice.
-
Edit claims in Search Results: Click this link to open the Search Results window. From this window you can go to the claim, the account, assign or unassign ownership, add or remove a tag, move to a collection agency, and adjust the balance.
Action buttons:
-
Move to collection agency: Click this button to move the claims to collections. You can select an existing agency or create a new one. When you send the account to a collection agency, the status of all the claims in patient billing for that account changes to "Closed - In collections." The write off amount displays on the "Move to collection agency" window. In addition, we add the collections agency as the final payer on the claim level COB. This allows you to post payments from the collections agency when they collect money.
-
Move to state debt collections: Click this button to move the account to state debt collections. Start by selecting the state from the drop-down list and clicking Confirm. After you click Confirm, the status for all claims in the account with the patient as the current payer changes to "Suspended – In state debt collections." The status is suspended (not closed) which means you don’t have to write anything off your books after performing this action. If the state collects from the patient, you can post the payment because the state is added as the final payer on the claim level COB.
-
Write off as bad debt: In cases where collection is not worth the effort or impossible to obtain, use the "Write off as bad debt" option. After you click Confirm, the status for all the claims associated with the account changes to "Closed – Balance resolved."
Some suggestions
If the account is not in collections, you can use a combination of the information from the "Patient responsibility" and "Running account balance" tabs to help make a determination on your next steps. Here are some examples:
- If the credit score is over 600 (high) with a high likelihood to pay, you may want to send another statement.
- If you are in the "Final statement sent" or "Other suspensions" tab and the number of sent statements exceeds the maximum number configured in the statement schedule, you can generate an additional statement by clicking the "Send another statement" button.
- If the income compared to FPL is low, you may want to contact the patient and see if enrollment in Medicaid is an option.
- If the credit score and likelihood to pay are low, and the patient has never made a payment, you may want to either move the account to collections or write off the balance as bad debt.
Patient statements
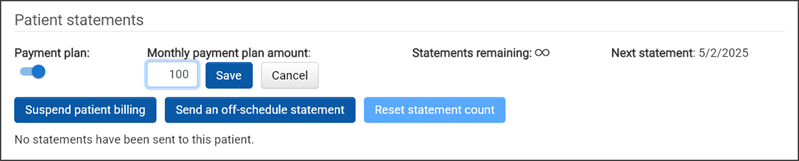
This small section is packed with functionality.
Payment plan: Use this section to turn a payment plan on or off for a patient account. Use the "Monthly payment plan amount" to set the dollar amount to be paid on a monthly bases. View how many statements remain and when the next statement will go out. To learn more, go to Patient Payment Plan.
Suspend patient billing: There are two ways an account can be suspended:
-
Automatically - Exceeds the number of sent invoices: The system suspends the account if the number of sent invoices is equal to or exceeds the value set in the statement schedule. When this is the case, the account displays under the "Final statement sent" tab on the Patient Billing page. To remove the suspension, click "Send another statement." This action removes the account from the list on the "Final statement sent" tab and changes the status on the claims associated with the account to "Queued for submission – Patient statement."
-
Manually – Biller suspended: A Biller can manually suspend the account because of an account review, when a patient address is needed, or when a patient is homeless, bankrupt, or sent a grievance.
When an account is manually suspended, the following things happen:
-
ZOLL Billing will no longer generate patient invoices on existing claims associated with this account. This is true even if the number of patient invoices has not exceeded the statement schedule.
-
ZOLL Billing will not generate patient invoices on future claims associated with this account. However, if the patient has insurance, the claim will still be sent to the insurance provider.
-
You can continue to post to this account
Note: Accounts that were suspended by the system display under the ‘Final statement sent’ tab. Accounts that were manually suspended by a user display under the ‘Other suspensions’ tab.
-
Send an off-schedule statement: Click this button to send another statement after a scheduled statement was sent.
Reset statement count: Click this button to reset the statement count for the patient account. For more information, see Resetting Patient Statement Counts.
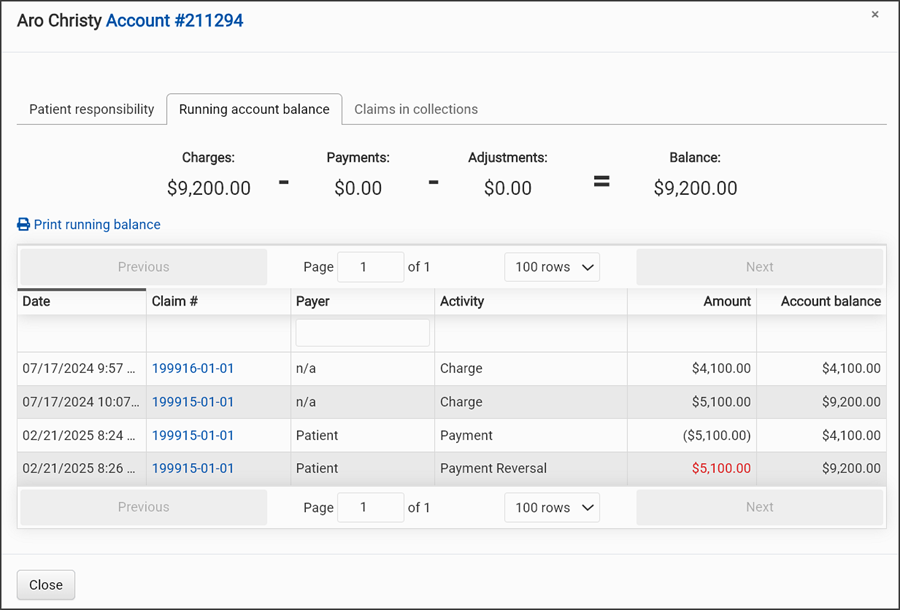
Running account balance
To view the patient's running account balance:
-
On the navigation bar, click Claims > Patient Billing.
-
Click the Active tab and then find the patient name on the list. If the list is long, start typing the name in the box under the Patient Name heading.
-
Click the Review icon
 under the Review column.
under the Review column. -
On the Patient Billing Review window, click the Running account balance tab.
-
Click the account number at the top of the window to view the patient's account page.
-
Click Print running balance to open a new tab that displays a PDF of the information shown in the tab. You can download or print the PDF.
-
Click the claim number to go to display that claim on the Claim page.
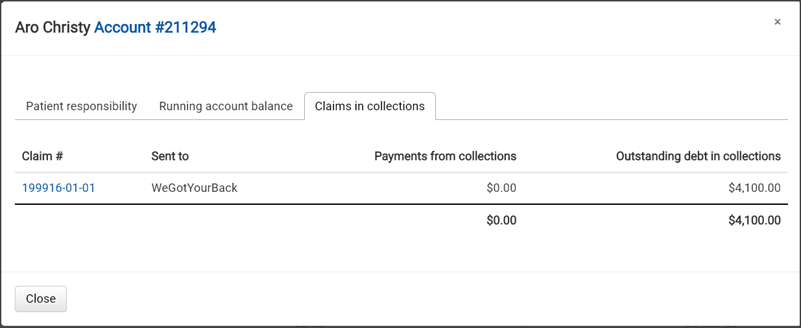
Claims in collections
To view the patient's claims that are in collections:
-
On the navigation bar, click Claims > Patient Billing.
-
Click the Active tab and then find the patient name on the list. If the list is long, start typing the name in the box under the Patient Name heading.
-
Click the Review icon
 under the Review column.
under the Review column. -
Click the Claims in collections tab. Note that if there are zero claims for this patient currently in collections, the tab will not be active.